
Pain tolerance: it’s a notion that often arises when discussing pain-inducing experiences amongst individuals. You may have recently undergone a painful root canal procedure, only to find that your friend who underwent the same procedure felt nothing at all. Maybe you had a tattoo done and were pleasantly surprised to find that you didn’t experience the degree of pain that your peers warned you about. This contrast is often chalked up to one’s high “pain tolerance” or “pain threshold.” These terms refer to varying and inconsistent degrees of pain that people experience when undergoing the same procedure, injury, or condition. Scientific studies have attempted to measure the factors that affect one’s pain threshold, including age, sex, and genetic ancestry. Aside from these biological factors, research has also been conducted to test the impact that sociological and psychological factors may have on pain perception. These factors include your support system, upbringing, mental state, and cognitive functions. Through such research, the scientific community has gauged the influence that emotion, cognition, and psychological state have on one’s perception of pain. We’ll be discussing how your body interprets and processes pain, and the role of psychology in pain management and perception.
The Scientific Mechanisms Behind Pain Perception

Pain is a complex and multifaceted experience. It is medically defined as an “unpleasant sensory and emotional experience associated with tissue damage. It allows the body to react and prevent further tissue damage.” Pain is a significant line of defense that the body activates when physical danger is perceived. When we cut our hand with a knife, we immediately experience a painful sensation that causes us to pull our hand away from the source of pain. While this reaction feels instantaneous and intuitive to us, many steps take place within our central nervous system that lead to this reactive outcome. Let’s take the knife-cutting example and break it down:
- While slicing an apple, you accidentally cut your finger with the knife. Your nociceptors (i.e., microscopic pain receptors located underneath the skin all throughout your body) sense the tissue damage.
- The nociceptors are now activated and must fire a response. They accomplish this by sending an electrical signal up the nerve fibers so that it reaches the spinal cord.
- These signals are then passed on from the spinal cord to the brain.
- Once the signal has reached the thalamus (the part of the brain that receives the majority of sensory information and serves as a relay station), it is then transmitted to other areas of the brain, including the somatosensory cortex (the part of the brain that receives and processes sensory information), the frontal cortex (the part of the brain that is responsible for higher cognitive functions), and the limbic system (the part of the brain that is involved in emotional and behavioral responses).
This process, though seemingly involved and extensive, occurs within a fraction of a second. Before the message even reaches the conscious areas of the brain, motor neurons have been activated to withdraw your finger from the mechanical stimulus (in this case, the knife). While this is our predictable physical response to pain, our psychological responses may vary greatly.
The Psychological Mechanisms Behind Pain Reception
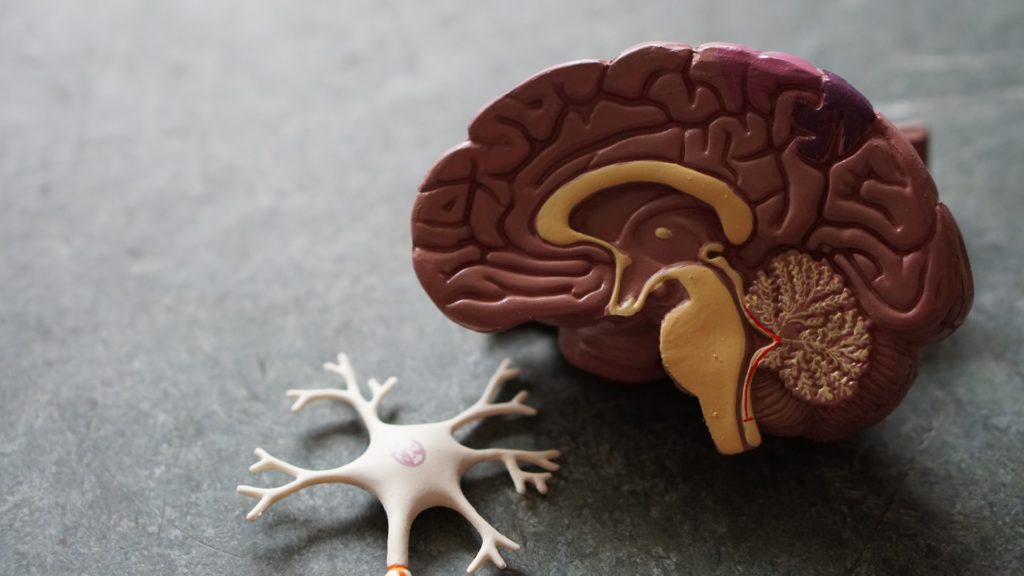
As we mentioned, pain signals are eventually sent to certain areas of our conscious brain that lead to less predictability in pain perception. Take, for example, the limbic system: this is the area of the brain that is responsible for memory storage and retrieval, along with emotional and behavioral responses. When the limbic system receives a signal indicating that there are pain-inducing stimuli present, the brain seeks to interpret and identify these stimuli. The limbic system may file through memories of previous knife-related injuries and compare those to the present injury. The same part of your brain will also dictate whether or not you become emotionally distressed, remain calm, or begin to cry. If you have previously experienced a very traumatic and/or painful knife injury, this will very likely influence how you interpret the pain this time around. The cut that you sustained this time around may be more shallow, and the knife may have caused objectively less tissue damage. However, the memory of a prior experience will influence your response.
Mental State and Mood

Another psychological factor that may determine the degree of pain you feel is your mental state. Say, for example, that you were fired from your job earlier today. You’re feeling slighted, angry, and are generally in a lousy mood. In the midst of this flare of negative emotions, you sprain your ankle. Your mood prior to sustaining the injury will influence how you ultimately interpret and perceive pain. One’s psychological state can also play a significant role in the outcome of pain treatment. Studies bolster the notion that patients entering pain treatment with an adverse mental or emotional state and minimal expectations of treatment success report higher degrees of pain and experience less relief from opioid analgesics. On the other hand, those entering treatment with a positive mental state and higher expectations of treatment success report lower degrees of pain and greater relief from analgesic administration.
Cognition & Distractive Tasks
Another factor that plays into pain perception is cognition. When a nurse administering an injection notices that their patient is nervous, they often use distractive tactics to minimize anxiety. This may include asking questions or engaging in an in-depth conversation. As the patient engages, they may not even be aware that the injection has already been administered. On the other hand, a patient that places their attention and focus solely on the injection taking place will most likely feel the needle make contact with their skin. They are more likely to perceive the process as more lengthy and uncomfortable than the distracted patient will. Studies that sought to define the relationship between cognition and pain have since demonstrated evidence that a patient’s pain perception may decrease when asked to complete cognitive tasks. This has led to distraction therapy being successfully employed as a coping strategy for pain management.
Chronic Pain
When we experience acute pain, the mechanisms behind it are quite simple. When a present stimulus causes real or potential tissue damage, this sensory information is sent to the brain. But how does acute pain evolve into chronic pain? This transition occurs when “repeated or continuous nerve stimulation precipitates a series of altered pain pathways, resulting in central sensitization and impaired central nervous system mechanisms.” The truth is that chronic pain is an extremely complicated condition that is often difficult to treat. Simply put, consistent or repetitive nociceptive stimulation can lead to changes in our pain pathways that result in central sensitization, and thus, chronic pain. While the dynamics of chronic pain have much of the medical community stumped, it’s believed that some people are more susceptible to developing chronic pain than others. In a study that set out to research the psychosocial factors that lead to the development of chronic pain, variables like childhood trauma, self-efficacy, and support systems were observed and shown to be contributory to persistent pain disorders. As more research is conducted, further risk factors will likely be identified to reduce the risk of chronic pain development.

The correlation between psychology and pain plays a major role in treatment outcomes and severity of perceived pain. In understanding that one’s emotional state and cognitive interactivity can increase or decrease pain perception, we have a much greater chance of achieving effective holistic pain management.
For more on pain management, check out MixPose’s targeted class schedule or try a personalized session with one of our instructors! Our daily yoga classes are led by skilled instructors, all of whom are qualified to help you modify yoga poses to appease any existing limitations or conditions you may have.


